What is the Gut Microbiome?
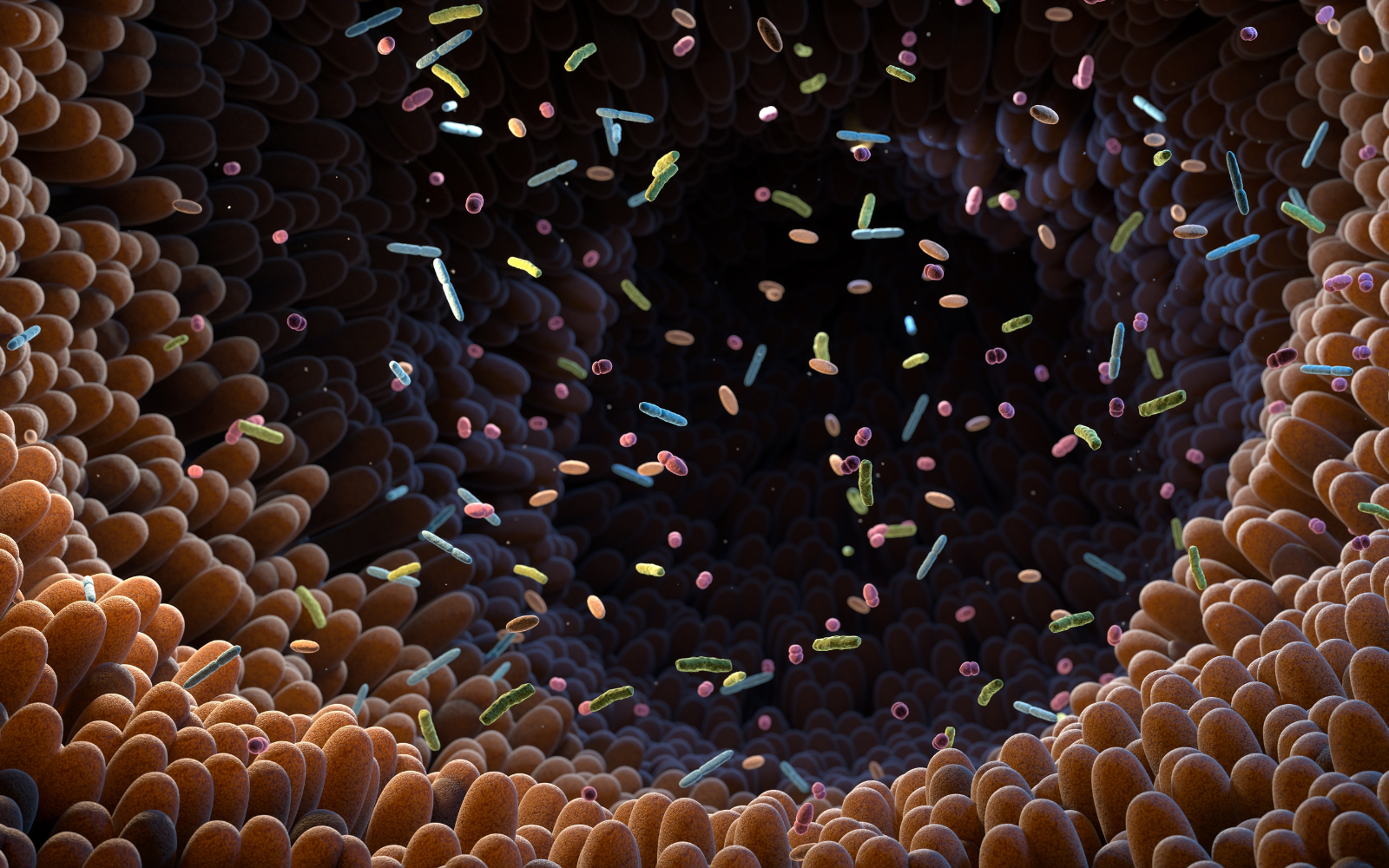
Your gut is populated by a combination of bacteria, archaea, and viruses, often referred to in combination as the gut microbiota. The microbiota of any two people will not be the same. The make-up of a person’s microbiota depends on genetic variants and other factors including ethnicity, dietary factors, lifestyle habits, and environmental conditions. Despite this variation, meta-analyses of thousands of peoples’ microbiota have revealed disease associations across pathologies and countries.
The gut microbiota evolved with humans in a symbiotic relationship. It is an essential part of our biology and supports many physiological functions like nutrient digestion and absorption, protection against pathogens, and production of essential metabolites like vitamins; helps maintain the integrity of our gut lining; and protects us from the diseases like obesity, cancer, and heart attacks.
Gut Dysbiosis, the 12th Hallmark of Aging
The gut microbiota also signal (talk to) to the peripheral and central nervous systems and other organs and strongly impacts the maintenance of whole body (host) health. If the communication between microbiota and host is disrupted due to imbalance in the microbiota, changes in functional composition or metabolic activities, or a shift in distribution, dysbiosis [1] occurs. Dysbiosis contributes to aging and a variety of pathological conditions including those listed above and more. As of 2023, it is now recognized as a key root cause of aging, known as the hallmarks of aging.
Microbiota Alterations in Aging
Bacterial diversity in the gut is established during childhood and remains relatively stable into adulthood. But, the architecture and activity of the bacteria undergoes gradual changes during aging, which eventually lead to a decrease in diversity.
Largescale studies of the gut microbiome and phenotypic data reveal that individual gut microbiomes become increasingly unique to each individual with age. In older age healthy individuals, their microbiome demonstrate this drift toward uniqueness, but this drift is reduced or absent in less healthy individuals.
Despite this uniqueness, when many thousands of peoples’ microbiota are examined, some trends are observed. For example, in healthy aging, there is a reduction of core gut bacteria like Bacteroides and Roseburia and an increase in other types of bacteria like Bifidobacterium and Akkermansia, which appear to have prolongevity effects [2]. Older adults have also been found to exhibit higher abundancies of several health-promoting bacterial species [3].
When the microbiomes of centenarians and supercentenarians are examined, however, they do not always follow the same rules as the general elderly population. For example, their microbiomes have shown enrichment of particular bacteria that generate secondary bile acids. Metabolizing these bile acids produced by the bacteria is hypothesized to reduce the risk of infection and contribute to intestinal homeostasis.
The microbiota have also been shown to produce other metabolites, which have been associated with different phenotypes (visible or observable traits). For example, p-cresol is correlated with increased frailty [4]. Conversely, certain indole metabolites are correlated with improved fitness in older adults and increased health and lifespan in mice [5]; this has been shown to be related, at least in part, through reducing inflammatory responses.
Fecal Microbiota Transplantations
Most health news enthusiasts have heard about fecal microbiota transplants (poop transplants). Whether you are intrigued or horrified at the thought, fecal microbiota transplants (FMT) have proven to be an effective treatment for C.diff in humans [6] and have revealed, at least in animal models, the role the gut microbiota play in aging and the maintenance of many different parts of the body including the brain and the ovaries.
FMT and Aging
Prematurely aged (progeria) mice exhibit intestinal dysbiosis characterized by an increase in the abundance of proteobacteria and cyanobacteria and a decrease in levels of verrucomicrobia [7]. Similarly, human progeria patients also exhibit dysbiosis. Long-lived humans, however, exhibit opposite effects to their gut microbiota with a substantial reduction in proteobacteria, for example, and an increase in verrucomicrobia.
When progeria mice were given FMTs from wildtype mice, the progeroid mice recipients had enhanced health and lifespans. Administering only the bacteria—verrucomrobium Akkermansia muciniphila—was also sufficient to obtain the same effects. FMT from progeroid to wild type mice, however, induced detrimental metabolic alterations. The effects of this FMT can be mitigated by restoring the secondary bile acids and other metabolites of the wildtype gut microbiota. These results suggest that restoring intestinal homeostasis—either by restoring bacteria levels or administering metabolites of those bacteria—can be sufficient to combat (premature) aging [7].
FMT and the Health of Systems
FMT has also revealed the role of gut microbiota in chronic systemic inflammation (another hallmark of aging), maintenance of brain health, and ovarian function and fertility: Gut dysbiosis plays a causative role in the chronic systemic inflammation and the decline in adaptive immunity associated with aging and age-related diseases. By transferring the gut mictiobiota of old mice to young mice [8], an inflammatory response is triggered; this response is characterized by enhanced CD4+T-cell differentiation in the spleen, upregulation of inflammatory cytokines, and increased circulation of inflammatory factors of bacterial origin. FMT from young mice donors to older mice reversed aging-associated differences in metabolites in the hippocampus and brain immunity and reduced aging associated impairments in cognitive behavior; this suggests that gut microbiota plays a role in the maintenance of brain health and immunity during aging [9]. FMT from young donor mice also improves ovarian function and fertility in mice [10]; when examined, the immune microenvironment of the aged ovaries is improved and the inflammatory markers are reduced.
Caloric Restriction & Gut Microbiota
Beyond poop implants, there have been a number of other prolongevity interventions on gut microbiota. One that can be taken on without a prescription or a PhD is caloric restriction. Restricting calories, more on this here, induces structural changes to the gut microbiome and increases the bacterial strains like Lactobavillus that influence healthy aging.
The Final Hallmark of Aging
This is the final hallmark set forth by Lopez-Otin et al in their updated 2023 paper on the Hallmarks of Aging [11]. It’s no wonder that gut dysbiosis was included. There are clear causal links between aging and dysbiosis. Interventions aimed at restoring a youthful microbiome, poop transplant and caloric restriction included, may extend lifespan and positively impact the health and functioning of other systems.
Spermidine, a natural polyamine, is believed to play an important role in gut microbiome regulation. Learn more about our premium food-derived spermidine supplement here.
References:
1. "What is Dysbiosis?" WebMD, 06 Dec. 2022, www.webmd.com/skin-problems-and-treatments/tc/athletes-foot-topic-overview.
2. "Gut Microbiota and Extreme Longevity" Current Biology, 12 May 2016, multiple authors.


Leave a comment
All comments are moderated before being published.
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.